Understanding Pressure Ulcers: Causes, Stages, and Prevention
Pressure ulcers, also known as bedsores or pressure sores, are a prevalent and potentially serious medical condition that affects individuals who are immobile or have limited mobility. These wounds develop when constant pressure, friction, or shear forces are applied to the skin and underlying tissues, resulting in damage and breakdown of the skin and underlying tissue. This essay aims to provide an in-depth understanding of how pressure ulcers occur, including their causes, stages, and preventive measures.
Causes of Pressure Ulcers
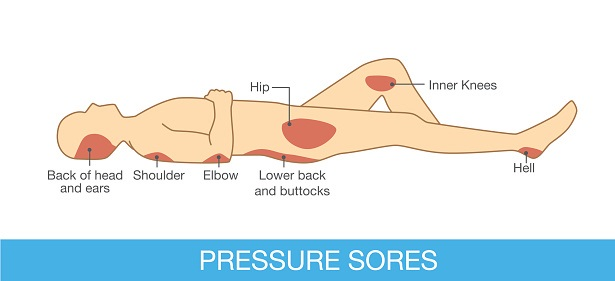
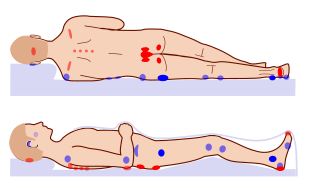
Pressure ulcers typically develop when prolonged pressure is exerted on specific areas of the body, primarily over bony areas or prominences. Individuals who are bedridden, wheelchair-bound, or have difficulty changing positions are at a higher risk to develop pressure ulcers. Common areas prone to pressure ulcers include the sacrum, heels, hips, elbows, and the back of the head. Factors contributing to the development of pressure ulcers include limited mobility, immobility, impaired sensation, poor nutrition, inadequate hydration, and moisture or friction on the skin.
Stages of Pressure Ulcers
Pressure ulcers are categorized into four stages, each representing the severity of the wound:
-
Stage 1
In this stage, the skin appears intact but may exhibit non-blanchable redness. The affected area may feel warmer or cooler compared to the surrounding skin.
-
Stage 2
In this stage, the skin breaks open, forming a shallow ulcer or blister. The area may be painful and exhibit redness, swelling, and a clear or yellow fluid discharge.
-
Stage 3
Stage 3 ulcers involve the deeper layers of the skin and may extend into the underlying subcutaneous tissue. The wound appears as a crater-like ulcer with significant tissue damage and may display signs of infection.
-
Stage 4
This stage represents the most severe form of pressure ulcers, involving extensive tissue damage that extends into muscle, bone, or supporting structures. The wound appears deep and may expose tendons, ligaments, or bone. Complications such as infections and necrotic tissue are common in stage 4 ulcers.
Understanding the Symptoms of Pressure Ulcers: Early Signs and Indicators
Pressure ulcers, also known as bedsores or pressure sores, are a significant health concern, particularly for individuals who are immobile or have limited mobility. Recognizing the symptoms of pressure ulcers develop pressure sores is crucial for early detection and prompt intervention. This essay aims to provide a comprehensive understanding of the symptoms of pressure ulcers and pressure sores, including the early signs and indicators that can help individuals, caregivers, and healthcare professionals identify and address these wounds.
The Initial Signs: In the early stages, pressure ulcers may exhibit subtle signs that should not be overlooked. It is important to pay attention to the following initial symptoms:

-
Skin Redness
One of the earliest signs of a pressure ulcer is persistent redness of the skin over a specific area. The affected skin may appear dusky, discolored, or have a bluish or purplish tinge. This redness is often non-blanchable, meaning it does not fade when pressure is applied and released.
-
Skin Temperature Changes
The skin over a developing pressure ulcer may feel warmer or cooler than the surrounding skin. Increased warmth can be an indication of inflammation, while decreased temperature may suggest compromised blood flow to the area.
-
Swelling or Edema
Edema, or swelling, may be present around the site of a pressure ulcer. This occurs due to fluid accumulation in the tissues as a result of impaired circulation and tissue damage.
-
Pain or Discomfort
In the early stages, a pressure ulcer may cause localized pain or discomfort. Individuals may experience tenderness, aching, or a sensation of burning or itching in the affected area.
Progression of Symptoms
As a pressure ulcer advances, the symptoms become more pronounced and indicative of underlying tissue of damage. It is essential to be aware of these progressive signs:
-
Blister Formation
As the pressure ulcer worsens, fluid-filled blisters may develop. These blisters can be painful, and the skin around them may appear further damaged.
-
Skin Breakdown
As the condition progresses, the skin over the pressure ulcer may break open, exposing the underlying layers of tissue. The wound may appear as an open sore or ulcerated area with visible tissue damage.
-
Foul Odor
Pressure ulcers at advanced stages can emit an unpleasant odor due to the presence of dead tissue and infection. This odor is often described as foul or putrid.
-
Deep Tissue Damage
In severe cases, pressure ulcers can extend into deeper tissues, affecting muscles, tendons, or even bone. The wound may become deeper and wider, and there may be a visible loss of tissue.
-
Signs of Infection
An infected pressure ulcer may exhibit signs such as increased pain, redness spreading beyond the immediate wound area, pus or drainage with an unpleasant odor, warmth, swelling, and the presence of fever or systemic symptoms.
-
Undermining or Sinus Tracts
In advanced pressure ulcers, the surrounding skin may show signs of undermining, which refers to the tunneling or erosion of tissue underneath the wound. Sinus tracts, small channels extending from the wound, can also develop.
Prevention of Pressure Ulcers
Preventing pressure ulcers is of paramount importance, particularly for individuals at increased risk. Several preventive measures can be implemented to minimize the occurrence of pressure ulcers:
-
Regular repositioning
Individuals who are immobile or have limited mobility should be repositioned frequently, ideally every two hours, to relieve pressure on vulnerable areas.
-
Maintaining skin hygiene
Keeping the skin clean and dry is essential in preventing pressure ulcers. Gentle cleansing and moisturizing can help maintain skin integrity.
-
Adequate nutrition and hydration
A well-balanced diet rich in nutrients, including protein, vitamins, and minerals, is crucial for maintaining healthy skin. Sufficient hydration is also important to prevent skin dryness.
-
Pressure redistribution surfaces
Utilizing pressure-relieving devices, such as specialized mattresses, cushions, or overlays, can help distribute pressure evenly and reduce the risk of developing ulcers.
-
Regular skin assessments
Conducting routine skin assessments allows for early detection of any changes or signs of skin breakdown. Prompt intervention can prevent the progression of pressure ulcers.
-
Education and training
Healthcare professionals and caregivers should receive education and training on pressure ulcer prevention, including proper positioning, skin care techniques, and identifying high-risk individuals.
-
Management of underlying medical conditions
Managing underlying conditions, such as diabetes, vascular diseases, or spinal cord injuries, can minimize the risk of developing pressure ulcers.

Treatment and Management
If a pressure ulcer does develop, timely and appropriate treatment is crucial to prevent complications and promote healing. Treatment options what is a pressure ulcer may include wound care, such as cleansing, debridement (removal of dead tissue), and the application of specialized dressings to promote healing. In more severe cases, surgical interventions may be necessary to remove necrotic tissue, close the wound, or reconstruct the affected tissue area.
Pain management, infection control, and addressing underlying medical conditions are integral components of pressure ulcer management. Healthcare professionals may prescribe pain medications, antibiotics for infection, and implement strategies to alleviate discomfort and facilitate healing.
Furthermore, multidisciplinary care teams comprising healthcare providers, wound care specialists, dietitians, and physical therapists collaborate to develop comprehensive care plans tailored to each individual’s needs. These plans may include nutritional support, physical therapy exercises, and ongoing wound assessments to monitor progress and adjust treatment as necessary.
The Importance of Education and Awareness
Education and awareness play a crucial role in preventing and managing pressure ulcers. Healthcare professionals should educate patients, caregivers, and the general public about the risk factors, preventive measures, and early warning signs of pressure ulcers. Understanding the importance of regular skin assessments, proper positioning, and maintaining overall health can empower individuals to take proactive steps in preventing pressure ulcers.
Healthcare facilities should also implement protocols and guidelines for pressure ulcer prevention, including staff training and adherence to best practices. Regular audits and quality improvement initiatives can help ensure compliance and provide ongoing education and support for healthcare providers.
Our Thoughts
Pressure ulcers are preventable wounds that occur due to prolonged pressure on the skin and underlying tissues. Understanding the causes, stages, and preventive measures is crucial in mitigating the risk of developing pressure ulcers, particularly for individuals with limited mobility or those who are bedridden. By implementing preventive strategies such as regular repositioning, maintaining skin hygiene, adequate nutrition, and appropriate support surfaces, the occurrence of these pressure injuries and ulcers can be significantly reduced.
In cases where pressure ulcers do develop, early detection and prompt treatment are essential for optimal outcomes. A multidisciplinary approach to wound care, including proper wound management, pain control, infection prevention, and addressing underlying medical conditions, is crucial in promoting healing and preventing complications.
Education and awareness among healthcare professionals, patients, and caregivers are fundamental in preventing pressure ulcers and ensuring timely intervention. By promoting best practices, implementing preventive measures, and fostering a collaborative approach to care, the burden of pressure ulcers can be minimized, leading to improved outcomes and enhanced quality of life for individuals at the risk of pressure ulcers.
Frequently Asked Questions
-
What is the primary goal of pressure ulcer treatment?
Answer: The primary goal of pressure ulcer treatment is to promote wound healing, prevent infection, relieve pain, and minimize complications associated with the ulcer.
-
What are the key components of pressure ulcer treatment?
Answer: The key components of pressure ulcer treatment include wound care, infection control, pain management, optimizing nutrition, and addressing underlying medical conditions that may hinder healing.
-
How is wound care performed for pressure ulcers?
Answer: Wound care for pressure ulcers involves cleaning the wound with a mild, non-irritating cleanser, removing necrotic tissue through debridement, applying appropriate dressings to promote a moist wound healing environment, and regularly assessing and documenting the wound’s progress.
-
What are the different types of dressings used for pressure ulcer treatment?
Answer: Various types of dressings can be used for pressure ulcer treatment, including hydrocolloids, foam dressings, alginate dressings, transparent films, and antimicrobial dressings. The choice of dressing depends on the characteristics of the wound and the healthcare professional’s judgment.
-
How is infection controlled in pressure ulcer treatment?
Answer: Infection control in pressure ulcer treatment involves proper wound cleansing, using topical or systemic antibiotics if an infection is present, and ensuring a sterile environment during dressing changes.
-
How is pain managed in pressure ulcer treatment?
Answer: Pain management for pressure ulcers can include the use of analgesic medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, as prescribed by healthcare professionals. Additionally, optimizing positioning and providing pressure relief can help alleviate pain.
-
Why is nutrition important in pressure ulcer treatment?
Answer: Nutrition plays a vital role in pressure ulcer treatment as it provides the necessary nutrients for wound healing. Adequate protein intake, along with vitamins and minerals, helps promote tissue repair and regeneration.
-
How is nutrition optimized for individuals with pressure ulcers?
Answer: Nutrition optimization for individuals with pressure ulcers involves collaborating with a registered dietitian who can assess nutritional needs, recommend dietary modifications, and provide appropriate supplements if necessary. This may include a high-protein diet, increased calorie intake, and specific nutrients like vitamin C and zinc.
-
What role do underlying medical conditions play in pressure ulcer treatment?
Answer: Underlying medical conditions, such as diabetes, vascular diseases, or immune disorders, can affect the healing process of pressure ulcers. Proper management of these conditions, including blood sugar control or vascular interventions, is important to facilitate healing and prevent recurrence.
-
When should surgical interventions be considered for pressure ulcer treatment?
Answer: Surgical interventions may be considered for pressure ulcer treatment in severe cases where conservative measures have been unsuccessful. Surgical options may include flap reconstruction, skin grafts, or debridement procedures to remove non-healing tissue and promote wound closure.
It’s important to note that the surgical treatment of pressure ulcers should be tailored to individual needs, and healthcare professionals should be consulted for proper evaluation and guidance.
